Abstract
Rationale
Nicotine and non-nicotine components of cigarette smoke contribute to its reinforcing effects; however, the specific role of each component in maintaining behavior has not yet been elucidated.
Objectives
To assess the reinforcing effects of nicotine and non-nicotine components of cigarette smoke by presenting a concurrent choice paradigm in which participants had access to intravenous (IV) nicotine infusions vs. saline (placebo) infusions and puffs from denicotinized (“denic”) cigarettes vs. air (sham puffs). We also measured the effects on self-administration of prior satiation with each component.
Methods
Sixteen smokers participated in seven sessions: 1) a baseline smoking assessment, used to tailor the nicotine dose per infusion; 2) two sessions for training discrimination of IV nicotine vs. saline infusions and denic smoke vs. sham puffs; and 3) four sessions assessing choice behavior after different satiation conditions.
Results
Denic smoke was self-administered more than any other alternative, including IV nicotine. IV nicotine, however, was preferred over IV saline and sham puffs. Preference for denic smoke vs. IV nicotine was inversely correlated with subjective ratings of “comfort” associated with nicotine. Smoke satiation reduced the number of denic puffs taken during choice periods, while prior nicotine administration did not affect puffing behavior. Smoking withdrawal symptoms were alleviated both by nicotine administration and by denic smoke.
Conclusions
In established smokers, non-nicotine aspects of cigarette smoking have potent reinforcing effects. While current smoking cessation pharmacotherapies primarily address the nicotine component of cigarette addiction, future cessation strategies should also be designed to target non-nicotine factors.
Similar content being viewed by others
Introduction
Cigarette smoking is a remarkably tenacious addiction, with relapse rates of greater than 90% on a given unaided quit attempt. Even with pharmacologic therapy, relapse rates often exceed 80% (Hughes et al. 1999). Such persistent behavior is indicative of powerful reinforcing mechanisms, yet there is only a partial understanding of the underlying processes that mediate the reinforcing effects of smoking. It is widely believed that nicotine is the primary reinforcing agent in tobacco, and that an important element of tobacco addiction comprises the euphoriant effects of nicotine, induced by stimulation of mesolimbic dopamine reward pathways (Balfour et al. 2000; Di Chiara 2000; U.S.D.H.H.S. 1988). However, nicotine, when administered apart from tobacco, often appears to have only weakly reinforcing properties. For example, unless engaged in a quit attempt, smokers uniformly prefer cigarette smoking to other forms of nicotine administration, including nicotine patch, gum, nasal spray, and inhaler.
A growing body of human research indicates that non-nicotine components of cigarette smoke play a major role in the reinforcing effects of smoking. For example, tobacco smoke presents numerous non-nicotine constituents, including monoamine oxidase inhibitors and acetaldehyde, which, alone or in interaction with nicotine, may be reinforcing (Rose 2006). In addition, smokers report enjoying the unique sensory attributes of cigarette smoke, including taste, olfactory and respiratory tract sensations. These cues likely serve as conditioned reinforcers contributing to the maintenance of addiction to cigarettes (Rose 2006; Rose and Levin 1991). Attenuation of these sensory components markedly reduces reported smoking satisfaction (Perkins et al. 2001; Rose et al. 1985, 1999b). Moreover, presentation of the sensory aspects of smoking elicits reports of satisfaction even when minimal doses of nicotine are delivered (Pickworth et al. 1999; Rose et al. 2000; Rose and Hickman 1987). Animal studies of nicotine self-administration have also shown that cues associated with nicotine intake have potent effects in terms of inducing high rates of operant responding (Caggiula et al. 2001; Donny et al. 2003; Goldberg et al. 1981), and that nicotine enhances the rewarding value of these cues. Thus, the self-administration of nicotine in the context of salient sensory cues may be critical for generating a powerful addiction.
An investigation of the interactions between nicotine and non-nicotine components of smoking may hold an important key for explaining the unique appeal of tobacco. Little is known, however, about how nicotine and non-nicotine components of cigarette smoking may facilitate or inhibit one another, as opposed to functioning as independent reinforcers. Although results from animal behavioral paradigms clearly show that nicotine potentiates the reinforcing effects of sensory cues (Donny et al. 2003), it is not clear whether administration of nicotine to human smokers potentiates the reinforcing effects of cigarette-related sensory cues (or non-nicotine smoke constituents). Conversely, it is not known whether presentation of non-nicotine smoke components affects the reinforcing value of nicotine.
The current study sought to characterize the separate and combined reinforcing effects of nicotine and non-nicotine components of smoking, using denicotinized cigarettes and intravenous (IV) nicotine administration to dissociate these two components. IV nicotine administration produces a similar arterial nicotine profile to that cigarette smoking (Rose et al 1999a). We quantified reinforcement by measuring smokers’ self-administration of IV nicotine infusions or puffs of denicotinized (“denic”) smoke, relative to appropriate sham or placebo controls, in a concurrent choice paradigm. Moreover, we assessed how satiation with either component affected self-administration behavior during subsequent choice periods.
In addition to behavioral measures, subjective effects of IV nicotine and denic smoke were also assessed to gain further clues about the potential complementary rewarding effects of nicotine and non-nicotine smoke components.
Methods
Subjects
Sixteen healthy male and female smokers were recruited from the community by newspaper and radio advertisements and by word of mouth. Subjects were between the ages of 18 and 55 and self-administered an estimated 10 mg or more of nicotine per day as estimated by the product of the number of cigarettes smoked daily and the FTC nicotine yields of their preferred brands of cigarettes, and scored ≥5 on the Fagerström Test for Nicotine Dependence (FTND), corresponding to moderate dependence (Fagerström et al. 1996). Subjects were screened to exclude serious medical conditions, based upon physical examination, ECG, serum chemistries, CBC, and urinalysis. Exclusion criteria comprised: uncontrolled hypertension (systolic >140 mm Hg, diastolic >90 mm Hg), hypotension (systolic <90 mm Hg, diastolic <60 mm Hg), coronary artery disease, cardiac rhythm disorder, any other major medical condition, current psychiatric disorder other than nicotine dependence, pregnancy or nursing, and current smokeless tobacco use. A negative drug screen for illicit substances was also required prior to entry into the study. Subjects were compensated $25/h for participation in the laboratory sessions.
Apparatus
Measurement of smoking topography
Smoking topography measures (puff volume, inter-puff time) were collected using the Clinical Research Support System (CreSS; Plowshare Technologies, Inc., Baltimore, MD). Subjects smoked all cigarettes through a mouthpiece that was attached to a laptop computer through a data collection interface. Expired air CO was also measured hourly using a Vitalograph CO monitor (Lenexa, KS).
Method of intravenous nicotine delivery
Pure nicotine base was obtained from Interchem Corp. (Paramus, NJ). A solution of 0.05% nicotine was prepared in saline, pH-adjusted to 7.0 using acetic acid, sterilized by filtration and autoclaving, and tested for pyrogens. A syringe pump (Harvard Apparatus Model 22 syringe pump, Holliston, MA) was used to deliver nicotine infusions; an identical apparatus was used to deliver saline. A saline drip was maintained in all conditions (approx. 2 ml/min), which served to convey any residual nicotine from the small dead space volume (approx. 0.8 ml) at the vein injection site.
The doses of nicotine administered in each pulsed IV injection were adjusted by dilution to be equal to the per-puff nicotine dose each subject obtained from their usual brands of cigarettes during ad lib smoking. This dose was calculated by manually drawing puffs from the same type of cigarettes (using a syringe), with the same average puff volume and inter-puff intervals that had been measured in an ad lib smoking baseline session. The smoke particulate matter was trapped in Cambridge filters (Paszkiewicz and Pauly 2008), and after extraction with ethanol, a spectrophotometer was used to measure the absorbance of the solution at a wavelength of 400 nm, a measure of “tar” concentration (Hinds et al. 1983). Using published values for the nicotine/tar ratio for each brand of cigarette (Federal Trade Commission 2000), the estimated nicotine delivery per puff was calculated.
Both visual cues (numerical values on computer display) and auditory cues (tone during pump activation) accompanied each self-administered dose of nicotine (or saline).
Cigarettes
Denic cigarettes were obtained from Philip Morris USA and delivered 0.08 mg nicotine and 9 mg tar (by FTC method).
Procedure
All procedures were reviewed and approved by the Duke University Medical Center Institutional Review Board, and written informed consent was collected from all participants prior to entry into the study. Participants were told that they may be asked to smoke cigarettes at specified times through a device that controlled the amount of smoke that could be inhaled. They were further instructed that these cigarettes might be denicotinized, i.e. “special cigarettes that do not contain nicotine.” They were also told that they might receive intravenous nicotine or saline.
The protocol entailed a total of seven sessions, each lasting approximately 4 1/2 h. Sessions were held in the morning after overnight (12 h) abstinence from smoking. Abstinence was confirmed by expired CO sampling (see below). All sessions took place with an IV line infusing either nicotine or saline. Table 1 depicts the study timeline, which is described in greater detail as follows:
Session 1 Smoking baseline assessment
Ad lib smoking of the usual brand was allowed (using the CReSS system). This session served to establish the dose of nicotine to be administered per infusion in subsequent sessions and the number of puffs and puff volume of denic cigarettes to be provided in the various satiation conditions (sessions 4–7);
Sessions 2–3: Training in self-administration procedure
The purpose of these two sessions (presented in counterbalanced order) was to train subjects to discriminate IV nicotine infusions from IV saline, and denic smoke from sham puffs. The onset of each series of puffs or injections was yoked to each subject's ad lib smoking in Session 1. For simplicity, the number of puffs or infusions presented in a given “bout” was set equal to the average number of puffs as that during ad lib smoking in Session 1, with the same average inter-infusion (or inter-puff) interval. The conditions were as follows:
-
a.
Training in self-administration of IV nicotine for 1 h 45 min, and self-administration of IV saline for 1 h 45 min. The training consisted of being instructed to press a response key for each dose according to the same schedule as puffs of cigarette smoke were self-administered during Session 1. Distinct keys, at the left and right margins of a computer keyboard, corresponded to the IV nicotine and IV saline infusions, with the positions kept consistent across sessions for each subject. The two arrangements, left-nicotine/right-saline and right-nicotine/left-saline, were counterbalanced across subjects, who were blinded to condition.
-
b.
Training in puffing denic cigarettes for 1 h 45 min and sham puffing for 1 h 45 min; sham puffing consisted of puffing on a cigarette using a special holder that blocked the smoke from the cigarette while allowing air to be taken into the mouth, with a draw resistance similar to that of a cigarette. As mentioned above, the number and timing of puffs were matched to Session 1.
Sessions 4–7: Self-administration assessment
The next four test sessions presented a 2 × 2 factorial design, assessing self-administration of IV nicotine infusions and denic puffs during choice periods that immediately followed programmed administration of one or both components. The following four conditions were presented in counterbalanced order:
-
a.
Programmed administration of puffs of denic cigarettes + IV nicotine (DENIC + IV NIC)
-
b.
Programmed administration of puffs of denic cigarettes + IV saline (DENIC + IV SAL)
-
c.
Programmed administration of sham puffs + IV nicotine (SHAM + IV NIC)
-
d.
Programmed administration of sham puffs + IV saline (SHAM + IV SAL)
The SHAM + IV SAL condition was intended to maintain a state of deprivation, whereas the other three sessions were intended to satiate participants with nicotine and/or smoke. During the programmed administration periods from 0–60, 70–130, and 140–200 min, the scheduled dosing condition was presented, using the rate of administration corresponding to that which each subject self-administered in Session 1. Choice periods allowing free access to selected alternatives were interspersed between the satiation periods, at 60–70, 130–140, and 200–210 min. During these choice periods, the reinforcing value of the various puffing and IV infusion alternatives was assessed. Specifically, the first two choice periods presented only two alternatives concurrently, assessing preference for denic vs. sham puffs, and preference for IV nicotine vs. IV saline infusions; the order of these two assessments was counterbalanced across subjects. The third choice period (200–210 min) presented all four alternatives concurrently (IV nicotine, IV saline, denic puffs, and sham puffs). During the choice periods, participants were able to control the number and pacing of puffs and infusions, and were not required to take any (Table 1).
Saliva samples were collected at the beginning of the session, then hourly until the end of the session. Heart rate and blood pressure were measured automatically every 5 min (Protocol Systems Inc., Beaverton, OR). Subjective measures of mood and smoking withdrawal were taken at the beginning of the session and approximately every hour thereafter, just prior to each choice period (see below).
Subjective measures
Withdrawal symptoms
Symptoms were assessed at each session using a modified Shiffman–Jarvik questionnaire (Shiffman and Jarvik 1976), containing scales for craving, negative affect, arousal, appetite, habit withdrawal, and somatic symptoms.
Cigarette and infusion evaluation questionnaires
Scales assessed satisfaction, psychological reward, nausea/dizziness, enjoyment of airway sensations, and craving reduction (Cappelleri et al. 2007; Rose et al. 2001). In addition, during sessions 2–3, subjects were asked to rate the nicotine content of the infusions.
Other subjective effects
Subjects were also asked to rate their mood states using several descriptors, including: “lightheadedness,” “pleasurable excitement,” “euphoria,” “dizziness,” “a feeling of comfort,” “a feeling of relaxation,” “nervousness,” “a sense of well-being,” “buzz,” “rush,” “high,” and “faintness”.
The following somatic symptoms were also assessed by self-ratings: “pain at the catheter/IV site,” “burning or pain in your arm,” “stomach ache,” “nausea,” and “headache”.
Saliva nicotine and cotinine concentrations
To confirm the systemic delivery of nicotine after IV administration, nicotine was assayed in saliva samples, thereby avoiding potential contamination of venous blood samples collected from the IV line that was used to administer nicotine. Moreover, data from the sham puffing satiation conditions were analyzed in order to avoid potentially confounding effects of nicotine directly entering saliva during smoking (even from denic cigarettes). Saliva nicotine concentrations are highly correlated with those of plasma and are approximately eight times higher (Rose et al. 1993). Samples were assayed by gas chromatography, using the method of Jacob et al. (1981), modified for use with a capillary column.
Expired air CO
To verify overnight abstinence, subjects’ expired air CO concentrations were measured using a portable CO monitor (Vitalograph, Inc., Lenexa KS). The criterion for assessing overnight abstinence was implemented using a formula that was derived on both theoretical and empirical grounds.Footnote 1 This formula assigned a threshold CO for each subject, which took into account the CO level measured in the afternoon, the estimated accumulation of CO during smoking the remainder of the day, and the half-life for elimination during the night (assumed to be 6 h). For a subject with an afternoon CO level of 30 ppm, a morning measurement of less than or equal to 20 ppm was required.
Data analysis
Behavioral preference was indexed by the number of puffs taken or injections self-administered during the choice periods. The first and second choice periods were analyzed separately from the third, because the first two periods presented a simple two-alternative choice between denic vs. sham puffs, or IV nicotine vs. IV saline, whereas the third choice period presented all four alternatives concurrently. The following questions were addressed:
-
1)
Were IV nicotine infusions more reinforcing than saline? The number of nicotine infusions was compared with the number of saline infusions, averaging across all four satiation conditions. Inspection of the values for the number of puffs or infusions self-administered showed highly skewed distributions, and therefore nonparametric Wilcoxon signed ranks tests were conducted.
-
2)
Were denic puffs more reinforcing than a) sham puffs and b) IV nicotine? The number of denic puffs was compared with the number of sham puffs, averaging across all satiation conditions.
The number of denic puffs was also compared with the number of IV nicotine infusions and sham puffs self-administered during choice period 3, which presented both denic smoke and IV nicotine alternatives along with the placebo/sham controls.
-
3)
Did the number of denic puffs or IV nicotine infusions selected depend on the prior satiation with nicotine or with denic smoke? The number of self-administered IV nicotine infusions (or denic puffs) was compared between the two conditions presenting IV nicotine satiation and the two IV saline conditions. Similarly, the two conditions presenting denic puffs as a satiation manipulation were compared with the two sham puff satiation conditions.
-
4a)
What subjective effects were elicited by presentations of IV nicotine or denic smoke?
Subjective ratings of mood and withdrawal symptoms in sessions 4–7 were analyzed in ANOVAs, with puff satiation condition (denic vs. sham puffs) and IV satiation condition (IV nicotine vs. saline injections) as factors, as well as their interaction. Ratings were analyzed from the 40-min timepoint in the satiation period, before choice period 1, in order to avoid any confounding effects of the puffs or nicotine obtained during the choice periods.
Prior to conducting ANOVA's on mood ratings, principal components analyses were conducted, with the goal of reducing the number of dependent measures by identifying combinations of intercorrelated items. This approach served both to limit Type I error by reducing the number of comparisons as well as reduce Type II error by increasing the reliability of the dependent measures (Cohen 1988). One principal components analysis was based on the differences in ratings between IV nicotine and saline conditions and a second analysis used the corresponding differences for the denic smoke and sham puffs. A root extraction method was used to arrive at a final number of factors, based on a “scree plot” (Stevens 1996). Two factors with substantial eigenvalues (>2) were obtained in both analyses, with excellent agreement in terms of the items loading on a given factor. The first factor, termed Euphoria, consisted of the following items: “euphoria,” “excitement,” “buzz,” “rush,” “high,” “nervousness,” “faintness,” “lightheadedness,” and “dizziness”. (The analysis of nicotine effects on Euphoria was also repeated using only the mood descriptors with clear-cut pleasant valence, i.e., “euphoria,” excitement,” “high,” and “rush” (cf. Dar et al. 2007), and the results were virtually identical to those described below). The second factor, termed Comfort, consisted of “comfort,” “relaxation,” and “well-being”. Intercorrelations between the two factors were low, approximately 0.3, and factors were uncorrelated with the withdrawal questionnaire scales. Factor scores were computed as the average of standardized variables (mean = 0, SD = 1).
For the cigarette and infusion evaluation questionnaires, data from sessions 2–3 were analyzed, because only infusions or only puffs were administered in each session (Fig. 1). Therefore, the ratings of puffs (or infusions) were not confounded by concurrent presentation of the other substance. Denic smoke was compared to sham puffs, and IV nicotine was compared to saline.
-
4b)
Were subjective effects correlated with behavioral preference?
To identify potential predictors of preference for the nicotine vs. non-nicotine aspects of smoking, we conducted simple linear regression analyses to relate nicotine preference to a number of candidate predictor variables. The dependent variable was the difference between the number of IV nicotine infusions, and denic puffs self-administered during choice period 3 (this variable proved to be normally distributed). Candidate predictor variables included: age, sex, FTND score, baseline number of cigarettes smoked daily, FTC nicotine yield of the preferred cigarette brand, and subjective ratings (collected prior to the first choice period). Subjective rating measures included the differences between DENIC + IV SAL and SHAM + IV NIC satiation conditions. Given the exploratory nature of these analyses, trends (p < 0.1), as well as statistically significant findings, are noted.
Results
Subjects
Six males (four Caucasian, two African American) and ten females (seven Caucasian, three African American) participated in the study. They had a mean age of 35.4 years (SD = 10.7), smoked an average of 25.2 cigarettes per day (SD = 11.1) with a mean FTC nicotine yield of 0.97 mg (SD = 0.25), had been smoking for 19.0 years (SD = 10.3), and their mean FTND score was 6.8 (SD = 1.5). Nine subjects reported a history of illicit drug use (six marijuana, two cocaine, and one unspecified). The rate of nicotine administration via IV infusion, which was set equal to subjects’ rates of nicotine intake when smoking their preferred brands of cigarettes, ranged from 0.6 to 1.9 mg in 180–510s, and the dose per infusion ranged from 0.05 to 0.21 mg.
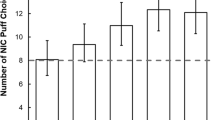
Choice behavior
Figure 1 depicts the frequency with which each alternative was selected during the three choice periods (averaged across satiation conditions). In the first two choice periods, the comparison of number of IV nicotine infusions vs. IV saline revealed a significant preference for IV nicotine (z = 2.55, p = 0.01). Likewise, subjects selected significantly more denic puffs than sham puffs (z = 3.10, p = 0.002). Preference for IV nicotine was associated with a history of illicit drug use (Mann–Whitney U = 11.5, p = 0.03). Interestingly, among those with a drug history (n = 9), the male subjects preferred IV nicotine to a greater extent than females. The difference in the number of IV nicotine and saline infusions ranged from 7 to 10 for males and 0 to 5 for females; Mann–Whitney test, z = 2.1, p = 0.04.
In choice period 3, the direct comparison between the number of denic puffs and IV nicotine infusions selected showed that subjects self-administered more denic puffs (z = 2.80, p = 0.005).
Effects of satiation manipulations on self-administration
The number of denic puffs taken during the initial two-alternative choice periods was not affected by prior satiation (ps > 0.1). However, an effect of satiation was detected on (four-way) choice period 3: as shown in Fig. 2, prior satiation with smoke, but not with nicotine, reduced the number of puffs taken (z = 2.86, p = 0.004).
Nicotine self-administration during all choice periods was unaffected by prior administration of nicotine or smoke (ps > 0.3).
Subjective ratings
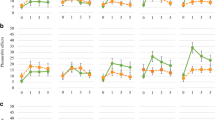
Withdrawal symptoms
Craving was reduced substantially by puffs of denic cigarette smoke (F(1,14) = 10.26, p = 0.006), see Fig. 3. There was also a trend for IV nicotine to reduce craving (F(1,14) = 3.17, p = 0.096), as well as an interaction of puff condition by IV condition (F(1,14) = 3.95, p = 0.07), such that the greatest reduction occurred in the combined denic smoke + IV nicotine condition.
Ratings of “habit withdrawal” showed a significant main effect of denic smoke to reduce withdrawal ratings, (F(1,14) = 6.15, p = 0.03), with no apparent effects of IV condition.
Negative affect ratings showed a significant puff condition X IV condition interaction, F(1,14) = 14.99, p = 0.002. Analyzed in terms of simple effects, each active treatment condition was able to relieve negative affect relative to the SHAM + IV SAL condition (F(1,14) = 7.13, p = 0.02 for DENIC + IV SAL; F(1,14) = 9.49, p = 0.009 for SHAM + IV NIC), but the two treatments together had less than additive effects.
Subjective arousal was increased by the denic smoke conditions relative to the sham control (F(1,14) = 6.19, p = 0.03), but there was no statistically significant effect of IV condition and no interaction.
No significant effects were seen for appetite, although there was a trend for the denic smoke conditions to reduce ratings (F(1,14) = 3.45, p = 0.08).
No effects were detected on any of the somatic symptom scales.
Cigarette and infusion ratings
Ratings in the sham puff and IV saline conditions were uniformly low, and the distributions were highly skewed. We therefore used nonparametric statistics (Wilcoxon signed ranks test) to compare conditions. Table 2 presents the median ratings for denic vs. sham puffs and IV nicotine vs. saline.
Ratings of satisfaction were significantly greater for smoke and for IV nicotine than their respective controls (z = 2.96, p = 0.003 for puff type; z = 2.83, p = 0.005 for infusion type).
Psychological reward ratings were also greater for smoke and for IV nicotine: (z = 2.81, p = 0.005 for puff type; z = 2.76, p = 0.0064 for infusion type).
Nausea/dizziness showed a trend for higher ratings in the smoke condition and significantly higher ratings after IV nicotine (z = 1.82, p = 0.07 for smoke; z = 2.38, p = 0.02 for nicotine).
Ratings of enjoyment of respiratory tract sensations were significantly higher in the smoke condition (z = 2.67, p = 0.007), with no significant effect of IV condition (z = 1.46, p = 0.14).
Craving reduction showed both an effect of smoke condition and IV condition (z = 2.67, p = 0.007 for smoke; z = 2.77, p = 0.006 for nicotine).
Subjects were able to discriminate between nicotine and saline infusions, with ratings of estimated nicotine content significantly higher for the nicotine infusions (z = 3.30, p = 0.0009).
Other subjective effects
Euphoria factor
There was a significant main effect of smoke condition, with ratings in the denic smoke conditions being higher than those in the sham puff conditions (F(1, 14) = 7.59, p = 0.02). There was also a trend for IV nicotine to increase Euphoria ratings (F(1, 14) = 4.17, p = 0.06). No interactions between puff condition and IV condition were noted. Mean factor scores in the four experimental conditions were: 0.44 (SD = 1.22) in the DENIC + IV NIC condition; −0.17 (SD = 0.45) in the DENIC + IV SAL condition; 0.12 (SD = 0.88) in the SHAM + IV NIC condition; and −0.32 (SD = 0.23) in the SHAM + IV SAL condition. The effect of IV nicotine on Euphoria was highly consistent within individuals. This intra-subject consistency was reflected in a high correlation between the effect of nicotine in the denic smoke conditions (defined as the difference between the DENIC + IV NIC and DENIC + IV SAL conditions) and the effect of nicotine as calculated based on the two sham puff sessions; r = 0.88, F(1,13) = 43.25, p < 0.0001.
Comfort factor
There were no statistically significant main effects of IV nicotine delivery or smoke condition (all ps > 0.2). However, as with Euphoria, there were highly consistent individual differences in the response to IV nicotine, with some participants reporting higher, and some lower, comfort in the IV nicotine conditions relative to saline. The correlation between the effect of nicotine in the denic smoke conditions and that in the sham puff sessions was highly significant; r = 0.75, F(1,13) = 16.62, p = 0.001. Interestingly, nicotine-associated Comfort (difference between IV nicotine and IV saline conditions) was highly correlated with the nicotine dose per infusion (r = 0.82, F(1, 13) = 26.05, p = 0.0002, excluding one outlier (in this analysis only) whose standardized residual was 6.2 standard deviations from the mean). Nicotine dose per infusion was also correlated with the denic-sham puff difference in Comfort ratings (r = 0.6, F(1,14) = 7.69, p = 0.01).
Subjects reported higher ratings in the IV nicotine (vs. saline) conditions for pain at the injection site (F(1,14) = 16.19, p = 0.001) and pain in the arm (F(1,14) = 24.07, p = 0.0003).
Predictors of preference for smoke vs. nicotine
The only demographic or individual smoker characteristic that was significantly correlated with preference for denic smoke vs. IV nicotine was a reported history of illicit drug use. For those reporting such a history (9 of 16 participants), there was less of a preference for denic smoke over IV nicotine infusions; F(1,14) = 4.56, p = 0.051. The mean difference (puffs–infusions) = 2.94 (SD = 1.42) vs. a mean = 7.46 (SD = 1.55) for those without a history. In both subgroups, however, puffs of denic smoke were chosen more often than IV nicotine infusions.
Importantly, reported pain at the IV site was not related to nicotine self-administration (p > 0.6). Other subjective effect ratings, however, were strongly correlated with choice behavior. Specifically, the difference in Comfort scale ratings between DENIC + IV SAL and SHAM + IV NIC conditions was highly correlated with preference of smoke over nicotine (r = 0.81; F(1,13) = 25.62, p = 0.0002); Figure 4 depicts the relationship between subjective Comfort ratings and preference for denic smoke vs. IV nicotine. There was a similar correlation, although less pronounced, between nicotine preference and the corresponding difference in ratings on the Euphoria scale (r = 0.56, F(1,13) = 5.90, p = 0.03). However, when ratings of both Comfort and Euphoria scales were entered into a multiple regression analysis, only the Comfort scale predicted choice behavior (F(1,12) = 12.57, p = 0.004); ratings of Euphoria did not (F(1,12) = 0.03, p = 0.9). The correlation between Comfort ratings and preference for smoke over nicotine appeared to be driven largely by the effects of nicotine on Comfort, as assessed by the mean difference in Comfort ratings between IV nicotine and IV saline conditions; r = .63, F(1,14) = 9.06, p = 0.009. The correlation between preference for smoke over IV nicotine and the difference in Comfort between denic and sham puffs was not significant (p = 0.9).
While the average nicotine dose per infusion was also modestly correlated with greater preference for nicotine (r = 0.53, F(1, 13) = 5.14, p = 0.04), when nicotine dose and Comfort ratings were entered into a multiple regression analysis, the only significant predictor was Comfort (F(1,12) = 20.94, p = 0.0004 for Comfort; F(1, 12) = 0.57, p = 0.46 for nicotine dose).
The correlation between behavioral preference and reported illicit drug use history remained statistically significant when Comfort ratings were included in a multiple regression analysis (F(1, 13) = 14.49, p = 0.002 for Comfort; F(1, 13) = 9.13, p = 0.01 for illicit drug history).
Physiological indices
Nicotine concentrations
The analysis of nicotine concentrations in saliva samples collected 40 min into the satiation period confirmed that the nicotine satiation manipulation affected systemic nicotine levels in the predicted direction; the mean saliva nicotine concentration was 362 ng/ml (SD = 350.9) in the SHAM + IV NIC vs. 61 ng/ml (SD = 62.6) in the SHAM + IV SAL condition (F(1,6) = 5.70, p = 0.05).
Cardiovascular responses
IV nicotine (vs. saline) administration significantly increased heart rate (mean = 77 bpm (SD = 10.8) vs. 69 bpm (SD = 11.4); F(1, 9) = 82.60, p < 0.0001) and diastolic blood pressure (66 mm Hg (SD = 8.4) vs. 62 mm Hg (SD = 8.2); F(1,10) = 6.06, p = 0.03), with a trend for increased systolic blood pressure (122 mm Hg (SD = 13.6) vs. 116 mm Hg (SD = 17.2); F(1,10) = 4.14, p = 0.07). Denic (vs. sham) puffs increased heart rate (mean = 76 bpm (SD = 11.5) vs. 70 bpm (SD = 11.2); F(1,9) = 8.10, p = 0.02), but did not affect blood pressure.
Discussion
The following discussion will be organized to address the questions posed in the Methods section.
-
1)
Were IV nicotine infusions more reinforcing than saline?
Participants preferred IV nicotine infusions over saline during the initial two-way choice periods. There has been little systematic research using IV nicotine administration since the early investigations by Henningfield and colleagues; they showed that rapid administration of high doses of IV nicotine (0.75–3 mg infused in 10 s) could maintain self-administration behavior, while eliciting positive, as well as negative mood effects (Henningfield et al. 1983). A more recent study (Harvey et al. 2004) was similarly limited by using unnaturalistic nicotine dosing parameters (0.75–3.0 mg in 10 s). Another study (Sofuoglu et al. 2008b) demonstrated preference for IV nicotine over saline at nicotine doses of 0.4 and 0.7 mg, but not at a 0.1-mg dose. Our study therefore fills an important gap in the literature by demonstrating the reinforcing properties of IV nicotine when it is presented in individually tailored, puff-sized doses.
-
2)
Were denic smoke puffs more reinforcing than a) sham puffs and b) IV nicotine?
A second key finding was that, remarkably, puffs of denic smoke were chosen more often than all other alternatives, including IV nicotine. Even in the SHAM + IV SAL condition, which did not provide any smoke or nicotine satiation (aside from the small amount self-administered in the first two choice periods), during choice period 3 very few IV nicotine infusions were taken. Less surprising was that denic smoke was preferred over sham puffs. It is noteworthy, however, that the act of puffing and inhaling per se had little reinforcing effect, as evidenced by the near-zero sampling of sham puffs during choice periods. These results support and extend recent demonstrations of the potent reinforcing effects of denic cigarettes in dependent smokers (Donny et al. 2007; Donny and Jones 2009), although denics are not as reinforcing as nicotine-containing cigarettes (Johnson et al. 2004). There are at least three aspects of denic cigarette smoke that may be reinforcing: 1) over a smoker’s history, the sensory cues presented in smoke (aroma, respiratory tract sensations) have become conditioned reinforcers through repeated pairing with nicotine administration (Rose and Levin 1991); 2) denic smoke contains pharmacologically active substances aside from nicotine; and 3) despite being “denicotinized,” these cigarettes contain a small amount of nicotine, which could occupy a substantial fraction of high-affinity nicotinic receptor binding sites (Brody et al. 2009). This factor, however, would not in itself explain the preference observed for denic smoke over nicotine itself.
-
3)
Was self-administration reduced by prior satiation? While satiation with denic smoke clearly suppressed subsequent choice for denic puffs during the third choice period, prior administration of IV nicotine had no apparent effect. This lack of a suppressive effect of prior nicotine administration contrasts with findings showing that IV nicotine administration diminishes ad lib smoking of nicotine-containing cigarettes (Lucchesi et al. 1967; Rose et al. 2003), although typically the magnitude of the suppression is only modest. In addition, some studies have reported that transdermal nicotine administration reduces ad lib smoking of denics (Donny and Jones 2009; Rose and Behm 1995), and in two previous studies we found that IV nicotine suppressed ad lib smoking of a denic when presented concurrently with puffing (Rose et al. 2003; Westman et al. 1996). Thus, any suppressive effect of nicotine on smoking of denics appears to be transient unless nicotine administration is maintained at a sufficiently high level.
In contrast to the partial satiation effect of denic smoke administration on puffing behavior, none of the satiation manipulations significantly affected IV nicotine self-administration. This apparent asymmetry suggests that any satiating effects of IV nicotine on subsequent nicotine seeking are modest and/or short-lived. Comparable results were also reported by LeSage et al. (2003), who, using a rodent IV nicotine self-administration paradigm, found that it required very high dose infusions of noncontingent IV nicotine—approximately seven times the level of voluntary intake—to attenuate nicotine self-administration behavior. Similar results in human smokers have also been reported by Dallery et al. (2003), who found that self-paced smoking of denic cigarettes had an equivalent satiating effect as did smoking nicotine-containing cigarettes; in contrast, after rapid smoking (three times the control rate) there was a more prolonged suppression of ad lib smoking by prior smoking of nicotine-containing cigarettes. The short-lived nature of satiation with normal rates of nicotine administration can be explained by the rapid decline in arterial nicotine concentrations within minutes after smoking (Benowitz et al. 1990), and/or a rapid recovery of nicotinic receptors from a desensitized state (Meyer et al. 2001).
The effects of the satiation manipulations were thus reflected most clearly in the suppression of puffing behavior by prior intake of denic smoke, as in a previous study (Rose et al. 2003). These results parallel findings from studies of other motivational states, such as food hunger and satiety, in which satiation with food preloads reduces the reinforcing value of peripheral food-related cues (e.g. taste), a phenomenon termed “aliesthesia” (Berridge 2004; Jiang et al. 2008). Moreover, as with IV nicotine self-administration in the current study, self-administration of the primary reinforcing substance is not well maintained when the usual peripheral sensors are bypassed, e.g., intragastric food delivery (Cabanac 1979).
-
4)
Subjective ratings and correlates of choice behavior. Subjective ratings provided important information about the qualitative nature of the complementary reinforcing effects of nicotine and non-nicotine smoke components. As in previous studies (Rose et al. 2000; Westman et al. 1996), denic smoke administration was associated with a robust alleviation of craving, negative affect, and habit withdrawal ratings. Somewhat surprisingly, it also increased ratings of euphoria. However, IV nicotine administration also reduced craving and diminished negative mood, and tended to increase ratings of euphoria and, in some participants, especially at higher doses, increased comfort. Comfort ratings were correlated, to a greater extent than euphoria, with behavioral preference for IV nicotine vs. denic smoke. The lack of correlation between comfort and withdrawal scale ratings suggests that the comfort scale tapped a unique and important mood dimension that may reflect the reinforcing effects of nicotine.
In addition to subjective ratings, a history of illicit substance use was also correlated with nicotine self-administration. Indeed, it has not been clearly demonstrated that nicotine self-administration occurs reliably in subjects without some illicit drug use history (although dependence is not a necessary condition (Sofuoglu et al. 2008b).
Clinical relevance
Our findings have the following potentially important implications for smoking cessation treatment or harm reduction strategies:
-
1)
The relationship between nicotine self-administration and effects on “comfort” challenges the view that tobacco addiction is mainly driven by euphoriant actions of nicotine. Consistent with this finding, smoking cessation treatment strategies that have attempted to replace these euphoriant effects by administering other psychostimulants, such as amphetamine, have proven unsuccessful. Indeed, a recent trial of the stimulant drug modafinil for smoking cessation was prematurely discontinued due to an exacerbation of withdrawal symptoms relative to placebo (Sofuoglu et al. 2008a). In contrast, preliminary work supports the potential efficacy of GABA-ergic sedative agents in the treatment of cigarette addiction (Smith et al. 1992).
-
2)
Further study of non-nicotine smoke components may lead to the development of methods for enhancing or prolonging satiety, thereby reducing the intake of toxic smoke constituents. For example, in one study, smokers were given low tar and nicotine cigarettes with capsaicin added to enhance sensory stimulation (Behm and Rose 1994). Smoke intake was significantly reduced relative to the control condition. Another strategy would be to provide non-cigarette substitutes that deliver appropriate peripheral sensory stimulation (Behm et al. 1993; Westman et al. 1995).
-
3)
By targeting non-nicotine aspects of smoking for therapeutic discovery efforts, more effective strategies for aiding smoking cessation may be discovered. Potential methods for devaluing or extinguishing smoking-related sensory cues include: a) the use of denic cigarettes for weeks leading up to the quit-smoking date (Becker et al. 2008; Rose and Behm 2004; Rose et al. 1998); b) aversive conditioning (Fiore et al. 2000); or c) removal of desired flavor constituents (e.g. menthol).
Study limitations
The present study, while contributing new findings relevant to tobacco addiction, had limitations. The preference shown for denic smoke over IV nicotine might have been influenced by participants’ unfamiliarity with the IV dosing procedure as compared with smoking behavior. Whether a longer exposure to self-administration of IV nicotine would result in a greater preference is an open question. IV nicotine also presented a mildly aversive stimulus, pain in the arm, which could have discouraged nicotine self-administration. However, pain ratings were not correlated with IV nicotine self-administration behavior.
Conclusion
This study achieved the primary goal of quantifying the relative reinforcing effects of nicotine and non-nicotine components in cigarette smoke. Our experimental paradigm utilized a unique approach to assess the reinforcing effects of nicotine dissociated from cigarette smoke, by administering cigarette puff-sized doses of nicotine. The results demonstrated the reinforcing effects of IV nicotine, and also identified a subjective mood variable, i.e., comfort, that was highly correlated with choice behavior. The results also add to a growing body of evidence showing that the non-nicotine aspects of smoking play a major role in motivating smoking behavior. In particular, denic smoke was more avidly self-administered than nicotine when the two alternatives were pitted against one another. Smoking cessation treatment approaches should address the role of these non-nicotine factors in order to achieve greater effectiveness than that attained using current therapies.
Notes
\( {\hbox{Criterion}}\,{\hbox{CO}} = 14 + {0.25 }\left( {{{1.33}}{\hbox{C}}{{\hbox{O}}_{\rm{aft}}} - 14} \right) \), where COaft refers to the afternoon CO reading.
References
Balfour DJ, Wright AE, Benwell ME, Birrell CE (2000) The putative role of extra-synaptic mesolimbic dopamine in the neurobiology of nicotine dependence. Behav Brain Res 113:73–83
Becker KM, Rose JE, Albino AP (2008) A randomized trial of nicotine replacement therapy in combination with reduced-nicotine cigarettes for smoking cessation. Nicotine Tob Res 10:1139–1148
Behm FM, Rose JE (1994) Reducing craving for cigarettes while decreasing smoke intake using capsaicin-enhanced low-tar cigarettes. Exp Clin Psychopharmacol 2:143–153
Behm FM, Schur C, Levin ED, Tashkin DP, Rose JE (1993) Clinical evaluation of a citric acid inhaler for smoking cessation. Drug Alc Depend 31:131–138
Benowitz NL, Porchet H, Jacob PI (1990) Pharmacokinetics, metabolism, and pharmacodynamics of nicotine. In: Wonnacott S, Russell MAH, Stolerman IP (eds) Nicotine Psychopharmacology. Oxford University Press, Oxford, pp 112–157
Berridge KC (2004) Motivation concepts in behavioral neuroscience. Physiol Behav 81:179–209
Brody AL, Mandelkern MA, Costello MR, Abrams AL, Scheibal D, Farahi J, London ED, Olmstead RE, Rose JE, Mukhin AG (2009) Brain nicotinic acetylcholine receptor occupancy: effect of smoking a denicotinized cigarette. Int J Neuropsychopharmacol 12:305–316
Cabanac M (1979) Sensory pleasure. Q Rev Biol 54:1–29
Caggiula AR, Donny EC, White AR, Chaudhri N, Booth S, Gharib MA, Hoffman A, Perkins KA, Sved AF (2001) Cue dependency of nicotine self-administration and smoking. Pharmacol Biochem Behav 70:515–530
Cappelleri JC, Bushmakin AG, Baker CL, Merikle E, Olufade A, Gilbert DG (2007) Confirmatory factor analyses and reliability of the modified cigarette evaluation questionnaire. Addict Behav 32:912–923
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Lawrence Erlbaum Associates
Dallery J, Houtsmuller EJ, Pickworth WB, Stitzer ML (2003) Effects of cigarette nicotine content and smoking pace on subsequent craving and smoking. Psychopharmacology (Berl) 165:172–180
Dar R, Kaplan R, Shaham L, Frenk H (2007) Euphoriant effects of nicotine in smokers: fact or artifact? Psychopharmacology 191:203–210
Di Chiara G (2000) Role of dopamine in the behavioural actions of nicotine related to addiction. Eur J Pharmacol 393:295–314
Donny EC, Jones M (2009) Prolonged exposure to denicotinized cigarettes with or without transdermal nicotine. Drug Alcohol Depend 104:23–33
Donny EC, Chaudhri N, Caggiula AR, Evans-Martin FF, Booth S, Gharib MA, Clements LA, Sved AF (2003) Operant responding for a visual reinforcer in rats is enhanced by noncontingent nicotine: implications for nicotine self-administration and reinforcement. Psychopharmacology (Berl) 169:68–76
Donny EC, Houtsmuller E, Stitzer ML (2007) Smoking in the absence of nicotine: behavioral, subjective and physiological effects over 11 days. Addiction 102:324–334
Fagerström KO, Kunze M, Schoberberger R et al (1996) Nicotine dependence versus smoking prevalence: comparisons among countries and categories of smokers. Tob Control 5(1):52–56
Federal Trade Commission (2000) “Tar’, Nicotine and carbon monoxide of the smoke of 1294 varieties of domestic cigarettes for the year 1998
Fiore MC, Bailey WC, Cohen SJea (2000) Treating tobacco use and dependence: clinical practice guideline. U.S. Department of Health and Human Services. Public Health Service, U.S. Department of Health and Human Services. Public Health Service
Goldberg SR, Spealman RD, Goldberg DM (1981) Persistent behavior at high rates maintained by intravenous self-administration of nicotine. Science 214:573–575
Harvey DM, Yasar S, Heishman SJ, Panlilio LV, Henningfield JE, Goldberg SR (2004) Nicotine serves as an effective reinforcer of intravenous drug-taking behavior in human cigarette smokers. Psychopharmacology (Berl) 175:134–142
Henningfield J, Miyasato K, Jasinski D (1983) Cigarette smokers self-administer intravenous nicotine. Pharmacol Biochem Behav 19:887–890
Hinds W, First MW, Huber GL, Shea JW (1983) A method for measuring respiratory deposition of cigarette smoke during smoking. Am Ind Hyg Assoc J 44:113–118
Hughes JR, Goldstein MG, Hurt RD, Shiffman S (1999) Recent advances in the pharmacotherapy of smoking. Jama 281:72–76
Jacob P, Wilson M, Benowitz NL (1981) Improved gas chromatographic method for the determination of nicotine and cotinine in biologic fluids. J Chromatogr 222:61–70
Jiang T, Soussignan R, Rigaud D, Martin S, Royet JP, Brondel L, Schaal B (2008) Alliesthesia to food cues: heterogeneity across stimuli and sensory modalities. Physiol Behav 95:464–470
Johnson MW, Bickel WK, Kirshenbaum AP (2004) Substitutes for tobacco smoking: a behavioral economic analysis of nicotine gum, denicotinized cigarettes, and nicotine-containing cigarettes. Drug Alcohol Depend 74:253–264
LeSage MG, Keyler DE, Collins G, Pentel PR (2003) Effects of continuous nicotine infusion on nicotine self-administration in rats: relationship between continuously infused and self-administered nicotine doses and serum concentrations. Psychopharmacology (Berl) 170:278–286
Lucchesi BR, Schuster CR, Emley GS (1967) The role of nicotine as a determinant of cigarette smoking frequency in man with observations of certain cardiovascular effects associated with the tobacco alkaloid. Clin Pharmacol Ther 8:789–796
Meyer EL, Xiao Y, Kellar KJ (2001) Agonist regulation of rat alpha 3 beta 4 nicotinic acetylcholine receptors stably expressed in human embryonic kidney 293 cells. Mol Pharmacol 60:568–576
Paszkiewicz GM, Pauly JL (2008) Spectrofluorometric method for measuring tobacco smoke particulate matter on cigarette filters and Cambridge pads. Tob Control 17(Suppl 1):i53–i58
Perkins KA, Gerlach D, Vender J, Grobe J, Meeker J, Hutchison S (2001) Sex differences in the subjective and reinforcing effects of visual and olfactory cigarette smoke stimuli. Nicotine Tob Res 3:141–150
Pickworth WB, Fant RV, Nelson RA, Rohrer MS, Henningfield JE (1999) Pharmacodynamic effects of new de-nicotinized cigarettes. Nicotine Tob Res 1:357–364
Rose JE (2006) Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl) 184:274–285
Rose JE, Hickman CS (1987) Citric acid aerosol as a potential smoking cessation aid. Chest 92:1005–1008
Rose JE, Levin ED (1991) Inter-relationships between conditioned and primary reinforcement in the maintenance of cigarette smoking. Br J Addict 86:605–609
Rose JE, Behm FM (1995) There is more to smoking than the CNS effects of nicotine. In: Clark PBS (ed) Effects of nicotine on biological systems II. Burkhäuser Verlag, Basel, pp 9–16
Rose JE, Behm FM (2004) Extinguishing the rewarding value of smoke cues: pharmacologic and behavioral treatments. Nicotine Tob Res 6:523–532
Rose JE, Tashkin DP, Ertle A, Zinser MC, Lafer R (1985) Sensory blockade of smoking satisfaction. Pharmacol Biochem Behav 23:289–293
Rose JE, Levin ED, Benowitz N (1993) Saliva nicotine as an index of plasma levels in nicotine skin patch users. Ther Drug Monit 15:431–435
Rose JE, Behm FM, Westman EC (1998) Nicotine/mecamylamine treatment for smoking cessation: the role of pre-cessation therapy. Exp Clin Psychopharmacol 6:331–343
Rose JE, Behm FM, Westman EC, Coleman RE (1999a) Arterial nicotine kinetics during cigarette smoking and intravenous nicotine administration: implications for addiction. Drug Alc Depend 56:99–107
Rose JE, Westman EC, Behm FM, Johnson MP, Goldberg JS (1999b) Blockade of smoking satisfaction using the peripheral nicotinic antagonist trimethaphan. Pharmacol Biochem Behav 62:165–172
Rose JE, Behm FM, Westman EC, Johnson M (2000) Dissociating nicotine and non-nicotine components of cigarette smoking. Pharmacol Biochem Behav 67:71–81
Rose JE, Behm FM, Westman EC (2001) Acute effects of nicotine and mecamylamine on tobacco withdrawal symptoms, cigarette reward and ad lib smoking. Pharmacol Biochem Behav 68:187–197
Rose JE, Behm FM, Westman EC, Bates JE, Salley A (2003) Pharmacologic and sensorimotor components of satiation in cigarette smoking. Pharmacol Biochem Behav 76:243–250
Shiffman SM, Jarvik ME (1976) Smoking withdrawal symptoms in two weeks of abstinence. Psychopharmacology 50:35–39
Smith MB, Brar SP, Nelson LM, Franklin GM, Cobble ND (1992) Baclofen effect on quadriceps strength in multiple sclerosis. Arch Phys Med Rehabil 73:237–240
Sofuoglu M, Waters AJ, Mooney M (2008a) Modafinil and nicotine interactions in abstinent smokers. Hum Psychopharmacol 23:21–30
Sofuoglu M, Yoo S, Hill KP, Mooney M (2008b) Self-administration of intravenous nicotine in male and female cigarette smokers. Neuropsychopharmacology 33:715–720
Stevens J (1996) Applied Multivariate Statistics for the Social Sciences. Lawrence Erlbaum Associates, Lawrence Erlbaum Associates
U.S.D.H.H.S. (1988) The health consequences of smoking: nicotine addiction. Office on Smoking and Health, Office on Smoking and Health
Westman EC, Behm FM, Rose JE (1995) Airway sensory replacement combined with nicotine replacement for smoking cessation: a randomized, placebo controlled trial using a citric acid inhaler. Chest 107:1358–1364
Westman EC, Behm FM, Rose JE (1996) Dissociating the nicotine and airway sensory effects of smoking. Pharmacol Biochem Behav 53:309–315
Acknowledgements
This study was supported by the National Institute on Drug Abuse grant DA02665.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rose, J.E., Salley, A., Behm, F.M. et al. Reinforcing effects of nicotine and non-nicotine components of cigarette smoke. Psychopharmacology 210, 1–12 (2010). https://doi.org/10.1007/s00213-010-1810-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-010-1810-2